Explain the steps involved in providing an intermittent enteral feeding – Delving into the intricacies of intermittent enteral feeding, this comprehensive guide unravels the essential steps and considerations involved in this specialized nutritional support technique, empowering healthcare professionals and caregivers with the knowledge and skills to deliver optimal care.
From patient preparation and tube insertion to formula preparation and post-feeding care, this guide navigates the complexities of intermittent enteral feeding, ensuring the safe, effective, and compassionate administration of nutritional sustenance.
Materials Required
Providing intermittent enteral feeding requires a comprehensive set of materials to ensure patient safety and comfort. These materials include:
- Feeding tube: A flexible tube used to deliver formula directly into the stomach or small intestine.
- Feeding pump: A device that controls the rate and volume of formula delivery.
- Enteral formula: A nutritionally complete liquid that provides essential nutrients to the patient.
- Syringes and needles: Used for administering medications and flushing the feeding tube.
- Stethoscope: For assessing bowel sounds and tube placement.
- Gloves: To maintain sterility and prevent infection.
- Tape or wrap: To secure the feeding tube in place.
Preparation
Proper patient preparation is crucial for successful intermittent enteral feeding. This includes:
- Assessing the patient’s nutritional status: Determine the patient’s calorie and nutrient requirements.
- Selecting the appropriate feeding tube: Consider the patient’s anatomy, underlying medical conditions, and duration of feeding.
- Obtaining informed consent: Explain the procedure and its risks to the patient and obtain their consent.
- Preparing the patient’s abdomen: Cleanse the insertion site and apply a topical anesthetic if necessary.
- Administering any necessary medications: Premedications such as antiemetics or sedatives may be required.
- Monitoring the patient: Monitor vital signs and assess the patient’s tolerance to the feeding.
Tube Insertion: Explain The Steps Involved In Providing An Intermittent Enteral Feeding
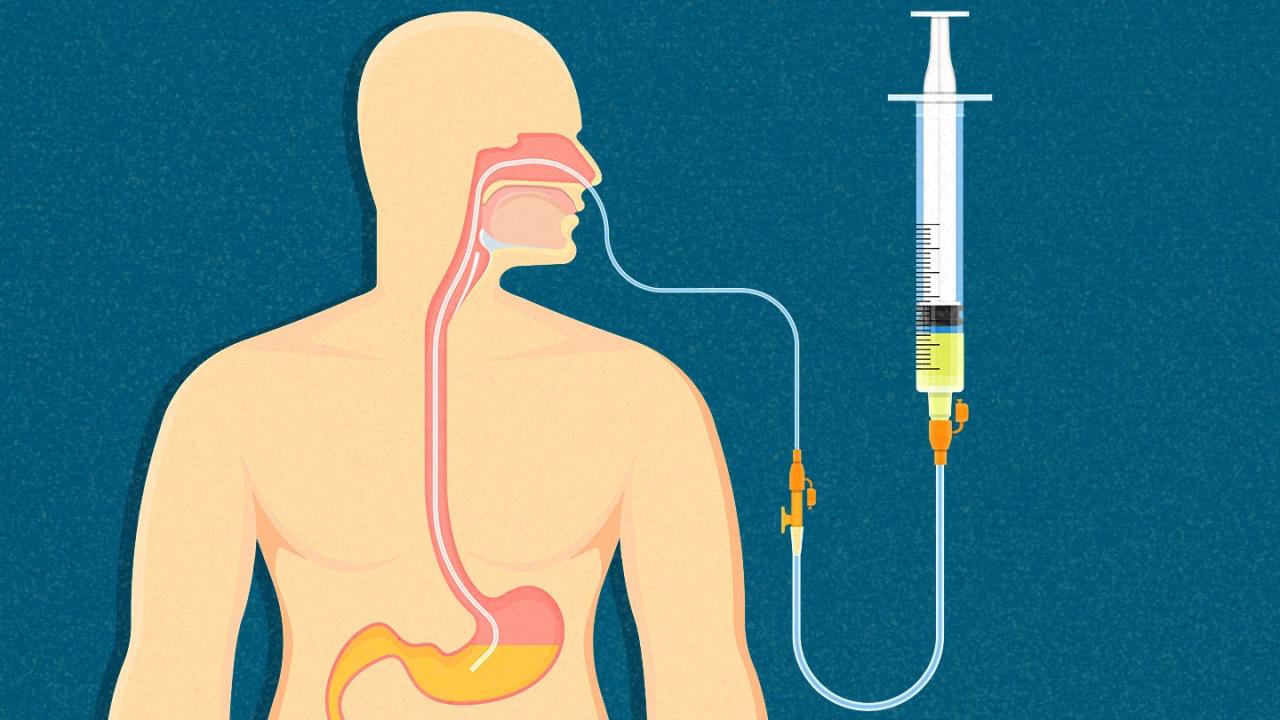
Tube insertion involves passing a feeding tube through the nose or mouth into the stomach or small intestine. There are different types of feeding tubes used, including:
- Nasogastric (NG) tube: Inserted through the nose and into the stomach.
- Nasoduodenal (ND) tube: Inserted through the nose and into the duodenum.
- Gastrostomy (G) tube: Surgically placed directly into the stomach.
- Jejunostomy (J) tube: Surgically placed directly into the jejunum.
The insertion technique varies depending on the type of tube used. Generally, the tube is measured to the appropriate length, lubricated, and gently inserted into the patient’s nose or mouth. The tube’s placement is then verified using a stethoscope or X-ray.
Formula Preparation

Enteral formulas are available in a variety of types, including:
- Standard formulas: Provide a balanced nutritional profile for most patients.
- Specialized formulas: Designed for patients with specific medical conditions, such as diabetes or renal failure.
- Elemental formulas: Broken down into small components for patients with impaired digestion or absorption.
The volume and concentration of the formula should be calculated based on the patient’s individual nutritional needs. Proper storage and handling of the formula are essential to prevent contamination and maintain its nutritional value.
Feeding Administration
Intermittent enteral feeding can be administered using various methods, including:
- Bolus feeding: A single large volume of formula is delivered over a short period of time.
- Cyclic feeding: Smaller volumes of formula are delivered at regular intervals throughout the day.
- Continuous feeding: A continuous flow of formula is delivered over a 24-hour period.
The method of feeding administration is selected based on the patient’s individual needs and tolerance. The feeding should be delivered at a rate that is comfortable for the patient and prevents complications such as nausea or vomiting.
Post-Feeding Care
Post-feeding care is essential to ensure patient comfort and prevent complications. This includes:
- Flushing the feeding tube: Flush the tube with water or saline after each feeding to prevent clogging.
- Caring for the insertion site: Clean the insertion site and apply a dressing to prevent infection.
- Monitoring the patient: Assess the patient’s tolerance to the feeding and watch for any signs of complications.
- Educating the patient and caregivers: Provide instructions on feeding administration, tube care, and potential complications.
Troubleshooting

Common problems that may arise during intermittent enteral feeding include:
- Tube displacement: The feeding tube may become dislodged or obstructed.
- Formula intolerance: The patient may experience nausea, vomiting, or diarrhea.
- Aspiration: Formula may enter the lungs, causing respiratory distress.
- Infection: The insertion site or feeding tube may become infected.
Troubleshooting these problems involves assessing the patient’s symptoms, identifying the cause, and implementing appropriate interventions. In some cases, seeking professional medical assistance may be necessary.
Documentation

Accurate documentation is essential for monitoring patient progress and ensuring continuity of care. This includes recording:
- Feeding times and volumes: Document the time, volume, and type of formula administered.
- Patient response: Note any signs of tolerance or intolerance, such as nausea, vomiting, or diarrhea.
- Tube care: Record any flushing or dressing changes performed.
- Patient education: Document any instructions provided to the patient and caregivers.
Electronic health records (EHRs) can be used to streamline documentation and improve communication among healthcare providers.
Popular Questions
What are the different types of enteral feeding tubes?
There are various types of enteral feeding tubes, including nasogastric tubes, nasoduodenal tubes, and gastrostomy tubes. The choice of tube depends on the patient’s individual needs and clinical condition.
How do I calculate the appropriate enteral formula volume and concentration?
The volume and concentration of the enteral formula should be determined based on the patient’s individual nutritional requirements and fluid needs. A healthcare professional should provide guidance on the appropriate calculations.
What are the potential complications of intermittent enteral feeding?
Potential complications include tube displacement, aspiration, gastrointestinal upset, and infection. Healthcare professionals should monitor patients closely for any signs or symptoms of complications.